

Other researchers have noted higher levels of positive end-expiratory pressure (PEEP) as a contributor to volutrauma. It was also reported7 that there was an increased incidence of extra-alveolar gas in patients requiring peak airway pressures of more than 40 cm H 2O. Haake et al9 reported volutrauma in 40 percent of their mechanically ventilated patients requiring peak airway pressures of more than 70 cm H 2O. Patients with lung conditions conducive to volutrauma (such as adult respiratory distress syndrome, aspiration pneumonia, and restrictive lung disease) may require higher peak airway pressures when volume-oriented ventilation is used, and may experience significantly higher incidence rates.7,10,11 Mechanically ventilated patients have been reported6-10 to experience a 4 percent to 15 percent incidence of pneumothorax.
#Barotrauma vs volutrauma professional
The professional literature has documented this phenomenon for more than 50 years.5 Inordinately large tidal volume delivery has been positively identified as a contributing factor in volutrauma.3,4 Once the gas has dissected the bronchovascular sheath, it then spreads throughout the thorax, manifesting itself as pneumomediastinum, subcutaneous emphysema, pneumopericardium, pneumoperitoneum, pulmonary interstitial emphysema, air embolism, and pneumothorax.
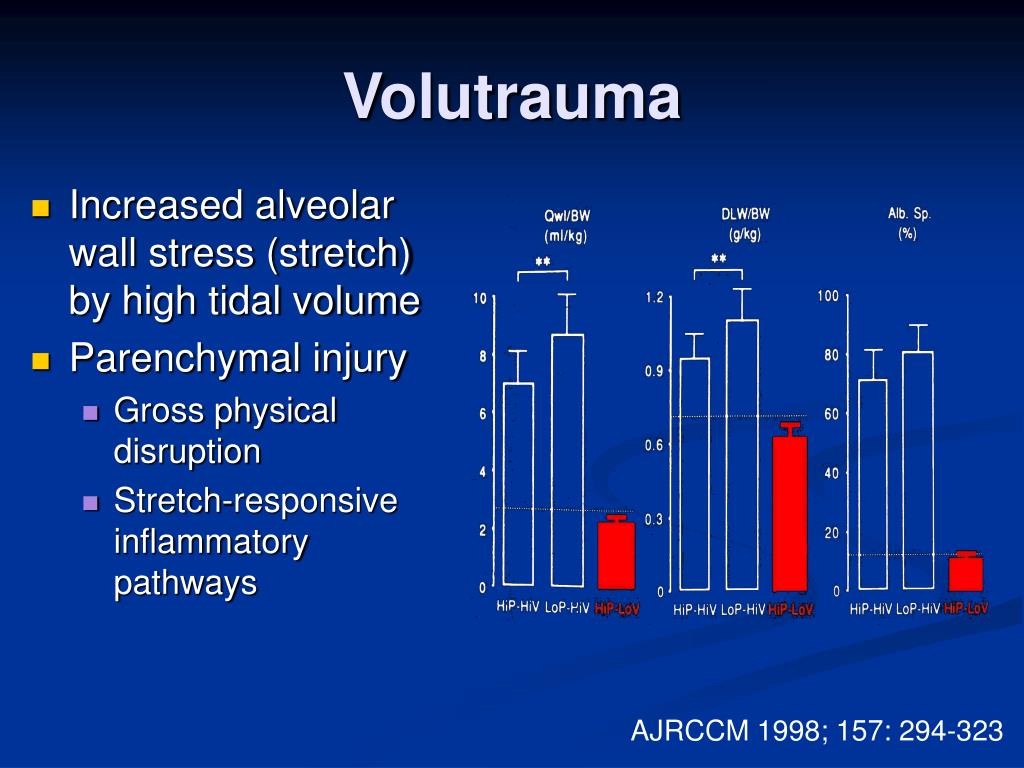
Recently, however, volutrauma has been proposed as a more appropriate term because it is now believed that overdistension of the lungs via excessive inflation volume is a more realistic explanation. In the past, the damage was thought to be the result of the application of excessive pressure commonly know as barotrauma.

The first reports of pulmonary volutrauma appears in the surgical literature.1,2 In more recent years, with the introduction of more sophisticated mechanical ventilators, a broader awareness of the many forms volutrauma may take has developed. This complication of mechanical ventilation may be transparent to the bedside clinician, as with pulmonary hyperinflation, or it may be life threatening, as in the case of untreated tension pneumothorax. This broad term is commonly used to define extra-alveolar air as it migrates from a ruptured alveolus into surrounding tissue spaces. One of the most frequently encountered complications of mechanical ventilation is volutrauma. If a patient should develop infection or experience volutrauma during the period of ventilation, the delay in extubation may be catastrophic, from both a physical and financial point of view. One of the more expensive procedures is mechanically ventilating a patient for prolonged periods. Managers must identify and track those diagnosis-related groups that have the potential to generate immense costs. Today’s respiratory care director must manage a department that is a cost center, not the revenue center of yesterday. Failure to detect this complication of mechanical ventilation can be catastrophic, from both a physical and financial viewpoint.


 0 kommentar(er)
0 kommentar(er)
